Research topics: Biomedical Signal Processing
Background
Cardiac arrest is the abrupt cessation of the mechanical activity of the heart, confirmed by the absence of circulation. It has a daily incidence of about 1000 in USA and in the EU. Survival to hospital discharge is extremely low, below 10% on average.
The field of resuscitation comprises all procedures aimed at reversing the cardiac arrest, restoring spontaneous circulation and breathing. In 1992, International Liaison Committee on Resuscitation (ILCOR) was formed to allow cooperation between the different resuscitation councils worldwide, such as the American Heart Association (AHA) and the European Resuscitation Council (ERC). Since 2000, researchers from the ILCOR have reviewed international science and knowledge in 5-year cycles to achieve a consensus on the science of resuscitation. This consensus makes possible to update the treatment recommendations described in resuscitation guidelines.
The ILCOR promulgates the concept of the chain of survival, a metaphor that describes the sequence of actions linking the victim of cardiac arrest with survival. It consists of four independent links:
- early recognition of the cardiac arrest and early activation of the emergency medical services
- early cardiopulmonary resuscitation (CPR)
- early defibrillation
- early advanced cardiac care.

Defibrillation consists in the passage of high-energy electrical current through the myocardium to terminate certain malignant arrhythmias and restore a perfusing rhythm.
Resuscitation guidelines describe how treatment should be provided by both the Basic Life Support (BLS) and the Advanced Life Support (ALS). BLS applies non-invasive care procedures to the patient, using automated external defibrillators (AEDs).
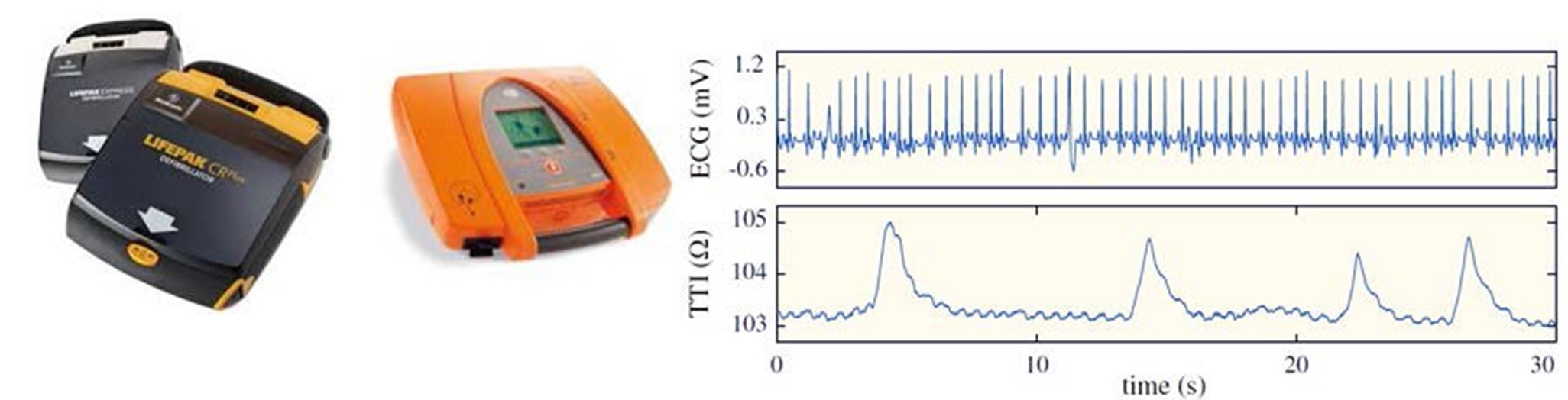
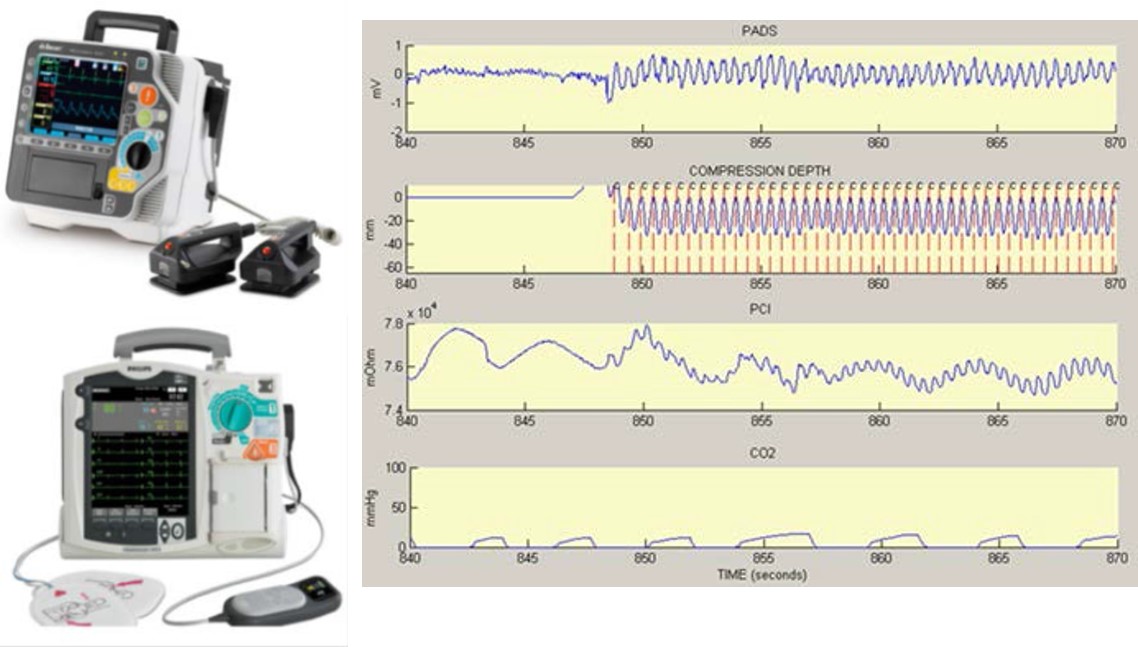
The ALS uses interventions and procedures performed or supervised by physicians. In addition to CPR and defibrillation, ALS uses airway management equipment (intubation, oxygen supply and capnographs) and different drugs administered through a venous line. Additionally, Additionally, ALS uses advanced devices for patient monitoring: monitor-defibrillators, capable of displaying and recording the signals that the specialist analyzes during the resuscitation attempt, including the ECG of up to 12 leads, the capnography signal, the pulse oximetry signal or the compression depth signal.
Activity of the group in this research topic
The GSC works has been working in the resuscitation field for 20 years, developing signal-processing techniques applied to different aspects of resuscitation:
- Algorithms for automated detection of shockable rhythms adapted for adult and pediatric patients.
- Diagnosis of the cardiac rhythm during ongoing chest compressions.
- CPR quality monitoring.
- Real-time systems to assist rescuers in the administration of chest compressions with the adequate depth and rate.
- Automated detection of patient’s restoration of spontaneous circulation.
- Advanced use of the capnography signal during resuscitation.
The extensive research work in this line has resulted in 6 doctoral thesis.
Currently, we are working on the analysis of the capnography signal. Current resuscitation guidelines emphasize the use of capnography by the ALS as a powerful non-invasive indicator of the hemodynamic response of the patient. However, the information provided by current capnographs during resuscitation (ventilation rate and end-tidal CO2 or ETCO2) is poor and inaccurate due to that chest compressions induce an interference on the capnogram, compromising the clinical interpretation of the procedure.
We believe that, in the future, capnographs will accurately measure ventilation rate and ETCO2 levels, even during chest compressions. Advanced capnographs will guide physicians on the quality of chest compressions, including depth, rate and impulsivity, so that the compression technique can be adapted to the patient's physical characteristics. In addition, capnographs will accurately alert the rescuer if the patient has recovered spontaneous circulation; and they will indicate to medical personnel the prognosis, favorable or not, of resuscitation efforts, trying to avoid the significant percentage of patients who survive but with severe neurological damage.
